Tinnitus, the ringing, buzzing or hissing sound of silence, varies from slightly annoying in some to utterly debilitating in others. Up to 15% of adults in the United States have tinnitus, and nearly 40% of those sufferers have the condition chronically and actively seek relief.
A recent study from researchers at the University of Michigan’s Kresge Hearing Research Institute suggests relief may be possible.
Susan Shore, Ph.D., Professor Emerita in Michigan Medicine’s Department of Otolaryngology and U-M’s Departments of Physiology and Biomedical Engineering, led research on how the brain processes bi-sensory information, and how these processes can be harnessed for personalized stimulation to treat tinnitus.
Her team’s findings were published in JAMA Network Open.
The study, a double-blind, randomized clinical trial, recruited 99 individuals with somatic tinnitus, a form of the condition in which movements such as clenching the jaw or applying pressure to the forehead result in a noticeable change in pitch or loudness of experienced sounds. Nearly 70% of tinnitus sufferers have the somatic form.
According to Shore, candidates with bothersome, somatic tinnitus, as well as normal-to-moderate hearing loss, were eligible to participate.
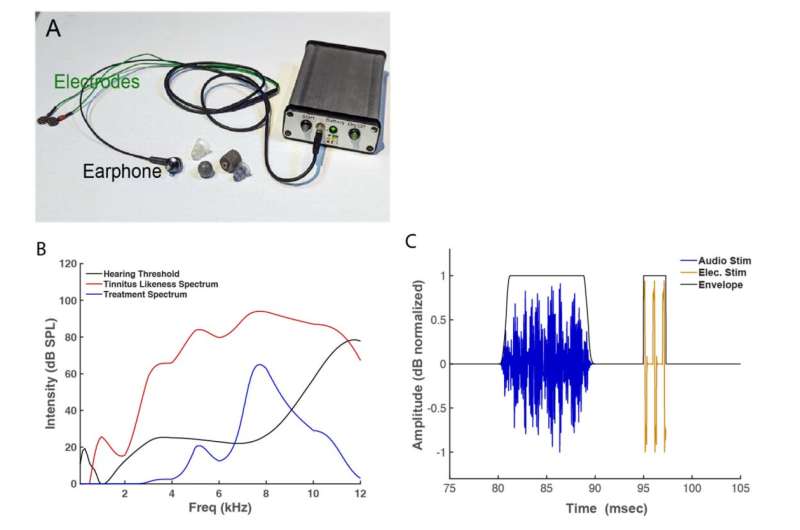
“After enrollment, participants received a portable device developed and manufactured by in2being, LLC, for in-home use,” she said. “The devices were programmed to present each participant’s personal tinnitus spectrum, which was combined with electrical stimulation to form a bi-sensory stimulus, while maintaining participant and study team blinding.”
Study participants were randomly assigned to one of two groups. The first group received bi-sensory (active) treatment first, while the second received sound-alone (control) treatment.
For the first six weeks, participants were instructed to use their devices for 30 minutes each day. The next six weeks gave participants a break from daily use, followed by six more weeks of the treatment not received in the beginning of the study.
Shore notes that every week, participants completed the Tinnitus Functional Index, or TFI, and Tinnitus Handicap Inventory, or THI, which are questionnaires that measure the impact tinnitus has on individuals’ lives. Participants also had their tinnitus loudness assessed during this time.
The team found that when participants received the bi-sensory treatment, they consistently reported improved quality of life, lower handicap scores and significant reductions in tinnitus loudness. However, these effects were not seen when receiving sound-only stimulation.
Further, more than 60% of participants reported significantly reduced tinnitus symptoms after the six weeks of active treatment, but not control treatment. This is consistent with an earlier study by Shore’s team, which showed that the longer participants received active treatment, the greater the reduction in their tinnitus symptoms.
“This study paves the way for the use of personalized, bi-sensory stimulation as an effective treatment for tinnitus, providing hope for millions of tinnitus sufferers,” said Shore.






Be First to Comment